Listen to this article
Narrated by Dr. Jana Rundle• 5.5 MB
Keyboard shortcuts: Space or K to play/pause • ← → to seek ±5s
You're scrolling through baby photos on your phone—those tiny fingers, that first smile—and the wanting hits you. You want another baby. You're ready. But then the memory surfaces: the fog, the crying, the feeling that you were drowning while everyone around you kept saying how "blessed" you should feel.
Your last postpartum experience was hard. Maybe it was postpartum depression. Maybe postpartum anxiety. Maybe both. And now that you're thinking about another pregnancy, one question keeps circling:
What if it happens again?
If you're carrying this fear, you're not alone. And I want you to know something important: Having had postpartum depression does increase your risk of experiencing it again—but it doesn't make it inevitable. And there's a lot you can do to prepare.
Understanding Your Risk
Let me be direct with you about what the research shows: If you experienced postpartum depression with a previous pregnancy, you have a 30-50% chance of experiencing it again. That's higher than the general population risk of about 15-20%.
Some women hear this and feel terrified. Others feel relief—because it means that 50-70% of women who had PPD don't experience it again with subsequent children.
Neither reaction is wrong. Both are understandable.
But here's what I want you to focus on: This risk isn't fixed. It's not a fate written in stone. Research shows that proactive intervention can significantly reduce your risk of recurrence. You're not powerless. You're actually in a position of advantage—because you know what to watch for.
What Makes Subsequent Pregnancies Different
Advantages You Have This Time
- You know the warning signs. You've lived through it. You know how it started, what it felt like, what made it worse.
- You can plan ahead. Unlike first-time parents who often don't know what hit them, you can build support systems before baby arrives.
- You have experience with recovery. You got through it once. You know it's survivable.
- You can advocate for yourself. You know you need monitoring and support, and you can communicate this to providers.
New Challenges to Consider
- You'll have a toddler or older child during pregnancy and postpartum. Sleep deprivation hits differently when you can't nap when the baby naps.
- Partner fatigue may be real. Your partner may feel anxious about going through this again too.
- You might minimize early symptoms ("I'm just tired from chasing a toddler").
- Guilt about impact on your older child if you do experience depression again.
Evidence-Based Prevention Strategies
Research by Dr. Michael O'Hara and colleagues has shown that certain interventions can meaningfully reduce PPD recurrence. Here's what the evidence supports:
1. Start Therapy Before Baby Arrives
This is one of the most powerful protective factors. Research shows that women who engage in preventive therapy during pregnancy—particularly interpersonal therapy (IPT) or cognitive behavioral therapy (CBT)—have lower rates of PPD than those who don't.
Think of it like physical therapy for a knee injury. You don't wait until your knee gives out again—you do strengthening exercises before the stress.
What this looks like:
- Meeting with a perinatal mental health specialist during pregnancy
- Identifying triggers from your previous experience
- Developing coping strategies specific to your situation
- Creating a postpartum monitoring plan
- Processing any remaining trauma from your previous postpartum experience
2. Talk to Your OB/Midwife and Psychiatrist Early
If you took medication during or after your last pregnancy, this conversation needs to happen before conception if possible, or early in pregnancy. There are decisions to make:
- Should you continue medication during pregnancy?
- Should you start preventive medication in the third trimester or immediately postpartum?
- What monitoring schedule makes sense?
Research from Massachusetts General Hospital shows that for women with a history of PPD, prophylactic antidepressant treatment (starting medication toward the end of pregnancy or right after delivery, before symptoms appear) can reduce recurrence rates.
This is a personal decision with no one-right-answer. But it should be a planned decision, not something you're figuring out in crisis mode.
3. Build Your Postpartum Support System Now
During pregnancy—not after birth—is the time to:
- Have honest conversations with your partner about what support looked like last time and what needs to be different
- Identify your village. Who can help with overnight duties? Who can take your older child(ren)? Who can bring meals?
- Hire help if financially possible. Postpartum doulas, night nurses, and mother's helpers aren't luxuries for high-risk mothers—they're prevention.
- Set boundaries with visitors who added stress rather than support last time
- Research childcare options for your older child(ren) so you're not figuring this out while sleep-deprived
4. Address Sleep Proactively
Sleep deprivation is one of the biggest triggers for mood episodes. This time, plan for it:
- Can you and your partner do shifts so each of you gets a 4-5 hour stretch?
- If breastfeeding, can you pump so someone else can do a feeding?
- Can you have help during the day so you can nap?
- Is there budget for occasional overnight help during the hardest weeks?
The goal isn't perfect sleep—that doesn't exist with a newborn. The goal is preventing the cumulative sleep debt that tips you into crisis.
5. Create an Early Warning Symptom Plan
Work with your therapist or provider to create a written plan that includes:
- Your personal warning signs (what appeared first last time?)
- When to increase support (e.g., "If I'm crying daily for more than 3 days...")
- When to contact your therapist
- When to contact your prescriber
- Emergency contacts and crisis resources
Share this plan with your partner. They may notice signs before you do.
What to Tell Your Partner
Partners who've supported someone through PPD often carry their own anxiety about another pregnancy. They may worry about:
- Seeing you suffer again
- Feeling helpless
- Managing everything while you recover
- Impact on your older child(ren)
- Whether the marriage can handle another difficult postpartum period
These are legitimate concerns, and they deserve space. Consider having a direct conversation (or several) that covers:
- What you both learned from last time
- What you'd do differently
- What signals should prompt action
- How to balance support for you with their own mental health
- Agreement that either of you can call for professional help without negotiation
The Reality: It Might Be Hard, And You Can Do It
I want to hold something complex with you: You might experience PPD again. Despite all your preparation, despite the therapy and the support systems and the medication decisions—you might still have a hard time.
And you can survive it.
You did it once. You know the terrain now. You know it's temporary. You know treatment works. You know you're not a bad mother.
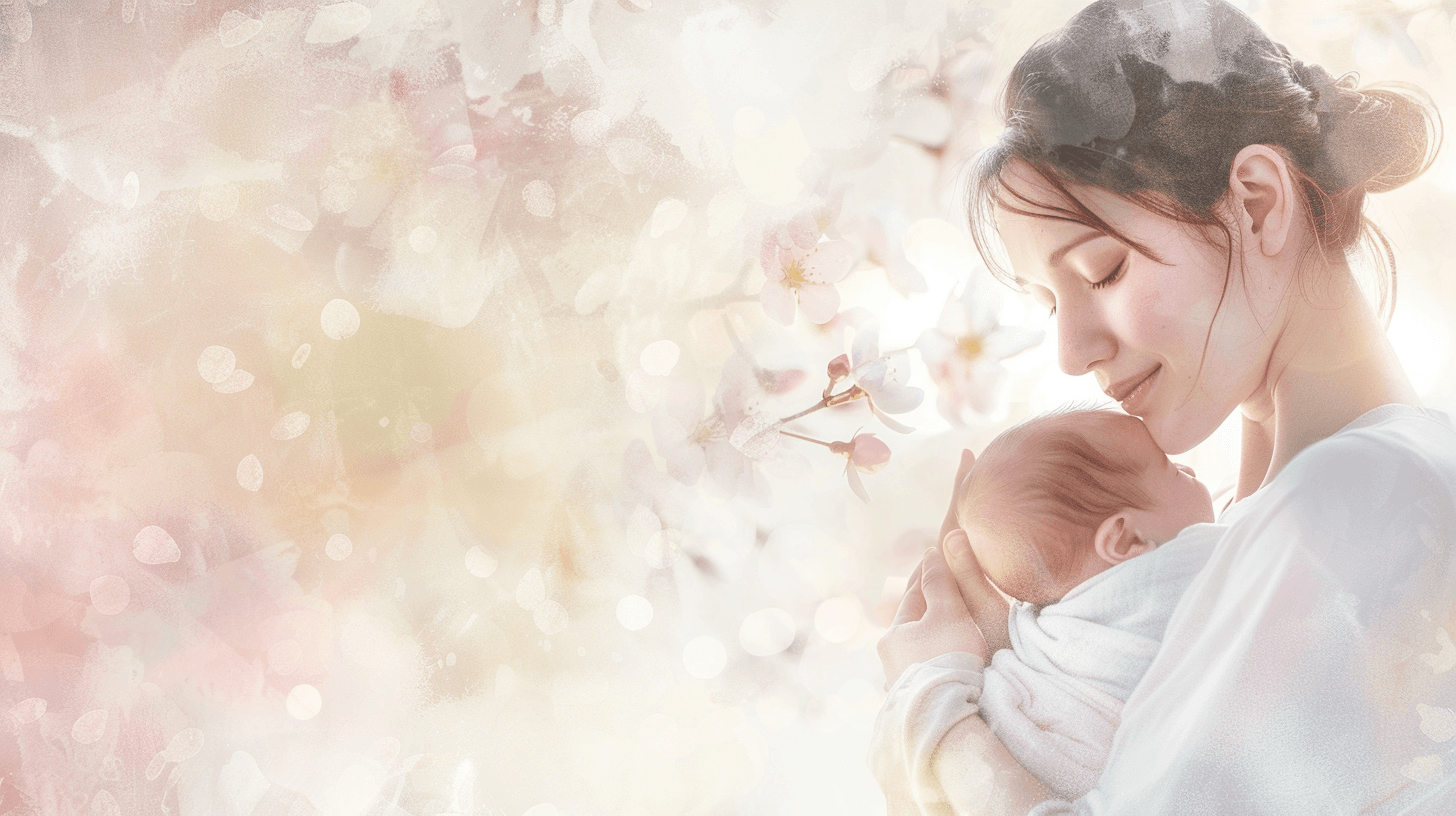
Many of my patients who experienced PPD with a second or third child say it was actually less severe—not because they were lucky, but because they caught it earlier, got help faster, and didn't waste months wondering if they were just "tired" or "ungrateful."
Some say their subsequent postpartum experiences were genuinely different—easier, more connected, even joyful. Not because they "fixed" themselves, but because they prepared.
Holding Both Realities
You can want another baby AND fear postpartum depression returning.
You can prepare thoroughly AND still not know exactly what will happen.
You can have increased risk AND still have excellent outcomes.
You can do everything "right" AND need help anyway—and that's okay.
The goal isn't to guarantee a perfect postpartum experience. The goal is to give yourself the best possible chance, with systems in place for if (and when) things get hard.
When to Start Preparing
Ideally: 3-6 months before you start trying to conceive. This gives you time to:
- Establish care with a therapist who specializes in perinatal mental health
- Meet with your OB or midwife to discuss your history
- Review medication decisions with a psychiatrist if relevant
- Process any unresolved feelings about your previous postpartum experience
If you're already pregnant: Start now. It's not too late. Any preparation is better than none.
If you're already postpartum: You know what to do. You've read the warning signs. Reach out for support today if you're struggling.
A Final Note
Some women decide, after their postpartum depression experience, that they don't want another pregnancy. That's a valid choice. PPD can be traumatic, and protecting yourself from that trauma is legitimate.
Other women decide the desire for another child is worth the risk, with preparation.
Neither choice is right or wrong. What matters is that it's your choice, made with full information and support.
If you're leaning toward another pregnancy, I hope this gives you a roadmap. You're not walking into this blind. You have experience, you have knowledge, and you have access to help.
That's not nothing. That's actually a lot.
Get More Like This
Join hundreds of moms receiving monthly mental health insights, evidence-based tips, and new articles.
No spam. Unsubscribe anytime.

Dr. Jana Rundle
Clinical Psychologist